We are so happy to be working with the Revenue Acceleration team. They get us the results we need for our revenue. We are a small agency, but they treat us as if we are their biggest client.
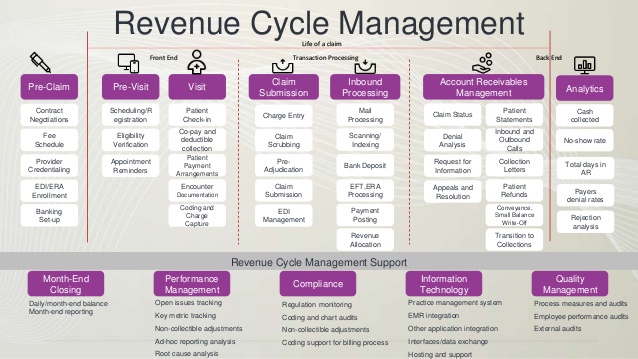
Our Services
- Eligibility & Benefits
- Monthly Census
- Referral entry
- Oasis Review (coding)
- Oasis Export
- Pre-Auth
- Billing
- Episodic & Non Episodic
- Denial Management
- AR follow up
- Appeals
- Payment posting
- Reporting